Add Power by Age: A Guide to Understanding Presbyopic Prescription Changes
- What is add power?
- The role of amplitude of accommodation (AoA)
- How add power changes with age
- How add power affects progressive lens design
- The Minkwitz Theorem
- Practical effect on lens designs
- Hard vs. soft progressive lens designs
- How to prescribe the right add power
- 1. Assess accommodative function
- 2. Analyze visual lifestyle demands
- 3. Consider patient history
- Common prescription challenges and solutions
- 1. Add power plateau
- 2. Rapid progression
- 3. Computer vision syndrome
- IOT optimizes patient outcomes through design and understanding
Add Power by Age: A Guide to Understanding Presbyopic Prescription Changes
Presbyopia is a predictable part of aging, but many eye care professionals struggle with determining the optimal add power for their patients. As the eye loses its ability to accommodate with age, patients require increasing levels of add power. However, while ECPs often use age as the primary linear factor for determining add power, there are actually more elements that contribute to it than just that. Modern lens designs go far beyond basic presbyopic prescription correction, and understanding the lens’ relationship with add power is the first step in choosing a prescription for a patient.
What is add power?
Add power represents the additional plus power needed to provide clear vision between the distance prescription and the near prescription for presbyopic patients. It compensates for the eye’s decreasing amplitude of accommodation (AoA), which typically starts declining noticeably in the late 30s or 40s and continues throughout life. This age is when most people’s crystalline lens becomes less flexible over time, and the ciliary muscle loses some of its effectiveness, creating the need for optical assistance to achieve clear near vision.
Add power is typically measured in quarter-diopter increments. For example, a patient with plano distance vision who requires +2.00D for comfortable reading has an add power of +2.00D. This additional power compensates for the eye's diminished ability to accommodate.
Presbyopic lenses add this plus power gradually in progressive lenses or a fixed segment with bifocal lenses. In PALs, the add power is blended along a vertical corridor, offering clear vision at all distances. However, as add power increases, this corridor becomes more complex to design due to unavoidable trade-offs in peripheral vision quality.
The role of amplitude of accommodation (AoA)
Accommodative amplitude is the maximum amount of accommodation a person can exert. AoA varies significantly between individuals of the same age, so while the average amplitude of accommodation provides helpful guidelines, measuring the individual’s accommodative ability leads to more precise prescriptions. The variation in accommodation between individuals is why age-based charts serve as starting points rather than definitive prescriptions.
How add power changes with age
The traditional understanding of presbyopic progression indicates a standard increase in add power with age. However, finding the right power requires a more nuanced approach that also factors in functional visual demands and individual accommodative patterns.
Historically, add power progression followed this general pattern:
| Age Range | Expected add power | Accomodative amplitude |
| 40-44 |
+0.75D to +1.00D |
3.5D to 4.5D |
| 45–49 | +1.25D to +1.50D |
2.0D to 3.0D |
| 50–54 |
+1.75D to +2.00D |
1.0D to 2.0D |
|
55–59 |
+2.25D to +2.50D |
<1.0D |
|
60+ |
+2.50D to +2.75D |
Nil |
Though a predictable starting point, research indicates that accommodative amplitude decline isn't perfectly linear. Factors like refractive error, occupational needs, lighting, and prior visual habits can shift the appropriate add power earlier or later. Some patients experience rapid changes over short periods, while others maintain relatively stable accommodation for years before experiencing more dramatic shifts. This variability highlights the importance of functional assessment over age-based prescription alone.
How add power affects progressive lens design

The Minkwitz Theorem
This theorem says that as power increases vertically down the corridor of a progressive lens, unwanted astigmatism off to the sides increases twice as fast. Mathematically expressed:
Astigmatism = 2(Add ÷ Progression Length)
The result is:
- Higher add = more peripheral aberration
- Shorter corridors = faster change = more noticeable distortion
Practical effect on lens designs
As a patient moves from a +1.50D add power to a +2.25D add power, they are not just “increasing strength”—they’re entering a completely different visual experience in the lens. The lens must compress more power change into the same vertical space, creating narrower intermediate zones and more peripheral blur.
The increased peripheral astigmatism requires different design strategies entirely:
- Longer progression lengths to reduce astigmatism buildup
- Modified blending techniques to manage peripheral aberrations
- Altered viewing zone proportions to maintain usable vision areas
- Different corridor geometries to optimize visual comfort
This explains why patients cannot receive the “same” progressive lens designs they previously had, and often report that the new lenses feel different from their previous pair. Although the lenses belong to the same design family, their optics and design have changed.
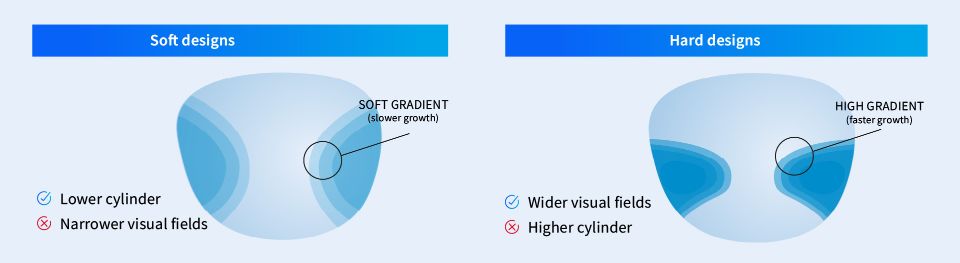
Hard vs. soft progressive lens designs
To combat the challenges of increasing add power, lens designers often shift between soft and hard design philosophies.
- Soft designs spread aberrations more gradually across the lens surface, making them easier to adapt to, which is ideal for early presbyopes.
- Hard designs localize power changes more aggressively to preserve wide near and distance zones, which is harder to adapt to but beneficial at higher add powers.
How to prescribe the right add power
Effective add power prescription requires balancing multiple factors: patient age, accommodative amplitude, visual demands, and lens design constraints.
1. Assess accommodative function
Though age is a strong predictor of add power, base your decision instead on the amplitude of accommodation. Determining the closest clear focus distance and when accommodation fails in daily activities, plus AoA, will create a well-rounded picture for determining add power.
A good rule to follow is that near vision requires about 2.50D of accommodation at 40cm. If a patient has only 1.50D of AoA left, they’ll need a +1.00D add power to compensate.
2. Analyze visual lifestyle demands
Different daily tasks demand different priorities in the near/intermediate/distance zones of a progressive lens. The visual requirements for patients who read novels, work at a screen all day, or spend most of their time driving are going to need different lens designs.
3. Consider patient history
If this is a patient’s first progressive lens, consider starting with softer designs and conservative add powers when possible. For example, a +2.00D add in a soft design adapts more easily than the same power in a hard design. If the patient is an experienced progressive lens wearer, then understand their current lens performance, any changes in accommodation since the last prescription, and any previous adaptation issues.
Common prescription challenges and solutions
Some patients may present visual factors that do not fall into the typical ‘easy to prescribe’ categories. Consider some common challenges when prescribing progressive lenses and add power.

1. Add power plateau
Some patients reach an add power level and seem to stabilize, showing no further accommodation decline for years. These patients may benefit from unchanged prescriptions, so don't automatically increase the add power based solely on age if the wearer reports continued satisfaction with their current correction.
2. Rapid progression
Occasionally, patients experience rapid accommodation decline, requiring significant add power increases over short periods. This may be caused by a medication, health changes, or dramatically increased near-work demands. These patients require careful management and may benefit from intermediate solutions during transition periods.
3. Computer vision syndrome
Patients reporting eye strain, headaches, or fatigue during computer use may not need higher add power but different add power distribution. Consider occupational lens designs that optimize intermediate vision, anti-fatigue lenses for early presbyopes, or blue light filtering in combination with appropriate add power.
Prescribing appropriate add power requires understanding the complex interplay between age, accommodation, lifestyle demands, and optical design constraints. While age provides a useful starting point, successful presbyopic correction depends on comprehensive patient assessment and thoughtful design selection.
IOT optimizes patient outcomes through design and understanding
Progressive lens design must evolve with increasing add power, making "the same design with more add" impractical. Instead, eye care professionals must consider how optical constraints change with add power and select designs accordingly. By aligning design with visual demands and physiological changes—not just a number on an age chart—eye care professionals give patients the clearest path to adaptation and comfort.
IOT uses a patient-centered approach grounded in optical science and experience to create lens designs that yield high satisfaction rates and successful presbyopic corrections.
If you’re ready to learn more about how these lens designs can improve your practice or lab portfolio, please get in touch.






