How Lens Innovations Are Changing the Game for Myopia Management
- Why myopia lenses are increasingly prevalent
- Lens innovations for myopia management
- Peripheral defocus lenses
- Why hyperopic defocus drives myopia progression
- How myopic defocus counters axial elongation
- Lenslets
- Concentric rings
- Orthokeratology contact lenses
- MyoLess: next-generation solution for myopia management
- Clinical Trial Efficiency
- Transitioning when myopia progression slows
- MyoLess lens and photochromic treatments
- Implementing advanced myopia management technologies
- Lab considerations for myopia spectacles
- Helping ECPs recommend the correct lens for myopia
- The future of spectacle lenses in myopia care
- Add freeform myopia lenses to your product line

How Lens Innovations Are Changing the Game for Myopia Management
Evolutionarily, humans have spent more time scanning the horizon, hunting, and spending whole days outdoors, so the eye adapted for this purpose. The relatively recent trend of spending more time indoors doing close-up work is impacting the eye in ways we are still uncovering. Researchers are learning more every day about how lifestyles impact vision and where myopia fits into that. What scientists know for sure is that if myopia trends continue, then we can expect half of the global population to be nearsighted by 2050.
This leaves the ophthalmic industry at a turning point, where spectacle lenses have rapidly evolved from passive vision correctors to proactive tools for managing myopia. Today, innovative spectacle lens designs not only correct refractive errors but also actively slow axial elongation. Combined with the latest technology, lenses for myopia management are a viable prescription for anyone experiencing symptoms and trying to slow the progression.
Why myopia lenses are increasingly prevalent
The global prevalence of myopia is increasing, particularly among school-aged children. While the precise mechanisms driving this trend are still under investigation, growing evidence suggests a strong correlation with shifts in behavioral and environmental factors. Increased time spent on near work (especially on digital devices) and reduced exposure to natural light are among the most frequently cited factors contributing to this issue.
Myopia, or nearsightedness, occurs when light entering the eye focuses in front of the retina, typically due to axial elongation or excessive corneal curvature. This causes distant objects to appear blurry while near vision remains clear. Though anyone can develop myopia, it most commonly presents in early childhood, stabilizing by adulthood. However, high myopia (≥ -6.00 D) can lead to complications like retinal detachment, macular degeneration, and glaucoma.
The rise of myopia underscores the growing need for proactive management strategies aimed at slowing its progression and reducing the risk of long-term ocular complications.
Lens innovations for myopia management
Advances in our understanding of peripheral retinal defocus and its influence on eye growth have opened the door to new strategies for managing myopia progression. Rather than simply correcting vision, today’s lens technologies are designed to help slow axial elongation in developing eyes.
As research continues to refine these mechanisms, manufacturers are developing increasingly sophisticated spectacle lens designs that not only improve visual acuity but also support long-term ocular health.
Peripheral defocus lenses
Peripheral defocus lenses introduce power to the periphery of the lens around a central clear zone. These use smooth, continuous power transitions to create a deliberate defocus zone (such as hyperopic or myopic defocus). This design mimics the therapeutic practice of signaling the eye to reduce axial elongation. Studies have shown that peripheral defocus lenses can reduce myopia progression by 50% in children.
Some peripheral defocus lenses retain a cosmetically clear appearance, making them appealing for patients and parents. They also allow labs to differentiate their product lines with clinically validated impact. Typical lenses in this portfolio could be lenslets, concentric rings, and custom designs like our MyoLess solution.
Why hyperopic defocus drives myopia progression
Hyperopic defocus occurs when light focuses behind the peripheral retina, which happens naturally in standard single-vision corrections. The eye interprets this as a “signal” that it is too short and responds by continuing to elongate. Over time, this axial elongation worsens myopia.
Research shows that this peripheral hyperopic blur is a key driver in the feedback loop between retinal defocus and ocular growth. Simply correcting central vision without addressing the peripheral retina inadvertently maintains this stimulus for elongation, explaining why single-vision lenses do not slow progression.
How myopic defocus counters axial elongation
Myopic defocus, in contrast, brings the focal plane in front of the retina in the peripheral field. This sends the opposite signal: that the eye is already long enough—or even too long—thereby reducing the stimulus for further growth. By creating a structured myopic defocus profile in the lens periphery, these lenses modulate the retina’s growth signals and slow axial elongation.
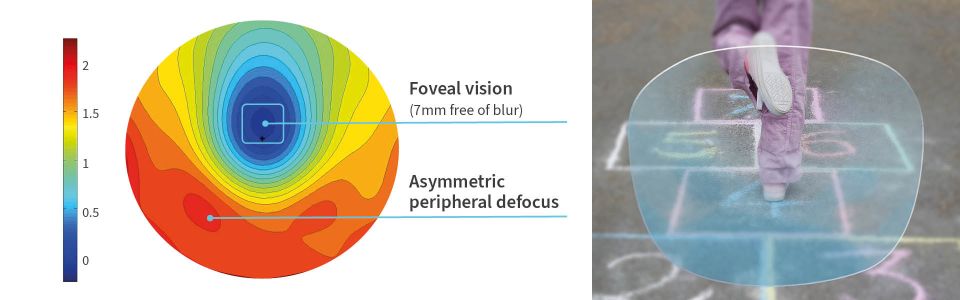
Emerging science further suggests that the retina responds asymmetrically. The nasal and temporal retina may have different sensitivities to defocus, which is why newer lens designs, such as MyoLess employ asymmetric defocus zones for optimized control.
Contributions of negative power
Recent studies have also explored the effect of negative power in peripheral zones, finding it may contribute to slowing axial elongation as well. While the dominant theory still favors positive peripheral defocus as the main mechanism, these findings hint that retinal blur may play a key role, though more research is needed.
Lenslets
Lenslet technology is one of the most widely studied approaches to delivering myopic defocus for myopia management. A lenslet is a microscopic segment with a fixed amount of positive power, which focuses light in front of the retina in the peripheral field. Instead of creating a continuous power gradient, some lenses incorporate hundreds of tiny lenslets across the peripheral zone of the lens surface. These lenslets form a subtle pattern around a central clear zone, maintaining clear distance vision while ensuring wearers benefit from the therapeutic effect of the peripheral defocus.
Clinical studies on lenslet-based designs, such as DIMS (Defocus Incorporated Multiple Segments) technology, have demonstrated strong efficacy in slowing the progression of myopia in children.
Concentric rings
Another approach to managing myopia progression is the use of concentric ring designs, which create alternating zones of clear vision and therapeutic defocus across the lens surface. These rings are arranged symmetrically around a central clear zone. Each ring incorporates a fixed positive addition power, generating peripheral myopic defocus while preserving functional vision in the intermediate areas.
The principle is similar to lenslets, as it introduces myopic defocus in the peripheral retina. However, instead of hundreds of micro-lenslets, concentric ring lenses typically use larger, smoother annular zones. Evidence from recent studies suggests that concentric ring or aspherical lenslet designs tend to produce lower contrast sensitivity loss and fewer visual artifacts than denser spherical‑lenslet ‘honeycomb’ arrangements. For example, a Frontiers 2024 study found that concentric rings with aspherical elements (Stellest) had significantly less impact on contrast sensitivity compared to honeycomb configurations of spherical lenslets.
One thing to consider is that concentric designs are symmetrical, so they don’t account for the retina’s nasal-temporal asymmetry, which research suggests plays a role in how the eye responds to defocus cues.
Orthokeratology contact lenses
Orthokeratology, also known as Ortho-K, involves wearing specially designed rigid gas-permeable contact lenses overnight to reshape the cornea temporarily. By gently flattening the central cornea and steepening the mid-periphery, Ortho-K corrects daytime vision without glasses while also inducing peripheral myopic defocus. This optical change helps slow the stimulus for axial elongation, making Ortho-K one of the most established contact lens options for myopia control.
However, Ortho-K requires strict hygiene, regular follow-up visits, and good compliance—factors that can be challenging for younger patients. While Ortho-K can be effective, it also carries a small but notable risk of corneal infection if not properly maintained. This is one reason many practitioners and parents prefer spectacle-based alternatives.
While lenslets, concentric rings, and Ortho-K have all demonstrated meaningful efficacy in slowing myopia progression, they also come with limitations, whether it’s manufacturing complexity, wearer adaptation challenges, or compliance demands. This has driven the development of next-generation spectacle lenses, which combine the proven principles of peripheral myopic defocus with a more sophisticated, retina-informed design that’s easier to prescribe, manufacture, and wear.
MyoLess: next-generation solution for myopia management
MyoLess lenses by IOT build on the well-established principle that peripheral myopic defocus slows axial elongation, but refines the approach with a more anatomically centered, wearer-friendly design. Unlike lenslet or concentric ring technologies, MyoLess features a central optical zone, about 7 mm wide, providing clear and stable vision for distance tasks.
Surrounding this zone is an asymmetric treatment area with carefully calibrated positive power: +1.8D on the temporal side, +1.5D on the nasal side, and +2.0D in the lower portion of the lens. This asymmetric configuration aligns with the natural nasal-temporal retinal differences, optimizing defocus exactly where the retina is most responsive.
A key differentiator is MyoLess’ flexibility in materials and prescriptions. Because it’s manufactured using freeform digital surfacing, the treatment zones are applied to the back surface of standard semi-finished lenses rather than requiring specialized blanks. This makes MyoLess available in a wide range of indexes, including CR-39, polycarbonate, and high-index materials, while remaining compatible with standard coatings like anti-reflective, UV protection, and scratch resistance. For labs and ECPs, this significantly reduces manufacturing complexity and cost while allowing for broader customization of different frame sizes and prescriptions.
MyoLess’ freeform digital surfacing technology also results in a smoother power transition that is invisible to the naked eye, maintaining a thin, lightweight, and cosmetically appealing lens. For the wearer, this means comfortable adaptation without the halos or ghosting sometimes associated with lenslet or concentric designs, making MyoLess a more appealing option for children to accept and parents to trust.
Clinical Trial Efficiency
A randomized, double-blind clinical trial conducted in a European population confirmed MyoLess as an effective myopia management solution.
After one year, children wearing MyoLess lenses showed a 39% reduction in axial elongation compared to those wearing standard single-vision lenses. After two years, the reduction remained significant at 29%, demonstrating robust efficacy even in a European population with lower baseline progression rates compared to those typically seen in Asia.

While the strongest effect occurred during the first year, which is common in all myopia control therapies, the trial confirmed that MyoLess performs comparably to other leading myopia control lenses, while offering superior material versatility and wearer comfort.
Transitioning when myopia progression slows
When myopia progression stabilizes following at least two years with no measurable change, patients can transition out of active myopia control lenses. For many, this means switching to a standard single vision lens solution, such as IOT’s Endless Single Vision. This step-down approach allows ECPs to simplify lens design and reduce cost while continuing to provide high-quality vision correction once active myopia management is no longer necessary.
MyoLess lens and photochromic treatments
While photochromic technology is not a myopia control treatment on its own, it can be an excellent complement to MyoLess lenses.
Photochromic lenses automatically darken in bright sunlight, providing comfortable vision while offering 100% UV protection. This added layer of protection supports overall ocular health, shielding young eyes from cumulative UV damage that contributes to long-term risks, such as cataracts and retinal degeneration. While outdoor time itself has not been shown to slow myopia progression in already-myopic children, it is widely recognized as protective for pre-myopes (and beneficial for overall health), delaying onset in those at risk.
When combined with the appropriate corrective lens, Neochromes are an example of a added value treatment that provides significant protective benefits supporting ocular health. For children spending time outdoors, Neochromes provide fast-reacting, high-performance photochromic activation, ensuring effortless transitions between indoor and outdoor environments.
By combining MyoLess lenses with Neochromes, ECPs can offer a single pair of glasses that manages myopia progression while also enhancing visual comfort and UV protection—an ideal all-day solution for active children.
Implementing advanced myopia management technologies
With such a new and diverse range of options for myopic patients, labs face the new challenge of manufacturing new technology, and ECPs need to know which lens designs to prescribe.
Lab considerations for myopia spectacles
Labs that embrace freeform myopia lenses are uniquely positioned to serve the next generation of ECPs and the millions of young patients needing tailored correction. Successfully producing these lenses requires a significant investment in advanced manufacturing capabilities, specifically freeform surfacing technology. Quality control systems also must be enhanced to verify the precision of microscopic lens elements and ensure consistent optical performance.
Helping ECPs recommend the correct lens for myopia
Wearer success with a lens begins with ECPs prescribing the correct lens design for the visual issue. As lens designs change and evolve, it’s important to make sure ECP partners understand the differences and use cases of each one. Labs and manufacturers can add real value here by providing:
- Decision-making tools to match lens designs to patient needs
- Usage guides for lens types by age, severity, or lifestyle
- Practice support in educating parents on the benefits of lens-based management
- Measurement tools such as axial length trackers, where applicable
The more intuitive and clinically relevant your product line is, the easier it is for ECPs to adopt and prescribe.
The future of spectacle lenses in myopia care
As global myopia prevalence increases, the role of myopia management lenses is expected to continue growing. What once was a basic corrective solution is now a customizable, tech-enhanced medical device. Researchers are exploring the combination of corrective lenses with newer therapies, such as bright light therapy and repeated low-level red light therapy, to achieve optimal results. With innovations like peripheral defocus zones, photochromic coatings, today’s lenses can impact visual acuity and long-term ocular health.
Add freeform myopia lenses to your product line
IOT Lenses delivers more than just progressive optics—we provide the complete toolkit for modern myopia management, including advanced lens designs and added-value solutions like Neochromes. Whether you're an in-house ECP lab or a wholesale manufacturer, we’re here to help you meet the future of eye care head-on.
Contact us to learn more about our lens designs portfolio and how it can benefit your practice or lab.